Breast reconstruction with prosthesis
Breast reconstruction is for patients who have had a breast removed, which is known as a mastectomy and is necessary for some forms of breast cancer.
Mastectomy can cause suffering and aesthetic and personal discomfort because of the importance of the breast in the image of femininity and the female psyche.
The objective of reconstruction is to reconstruct a breast that looks as natural as possible, aiming to restore symmetry and in keeping with the patient's physique.
The immediate reconstruction is performed in the same time as the mastectomy.
Secondary reconstruction is carried out, along with the complementary treatments that are required, after the mastectomy.
However, breast reconstruction is not compulsory as an external prosthesis can be worn inside the bra and this may be sufficient for some patients who do not wish to have another operation after the mastectomy.
For patients who want reconstruction, the simplest method is to reconstruct the breast by inserting a prosthesis.
There are many models of prostheses with different materials, content, volume, shape and projection to suit each individual patient’s anatomy. In the majority of reconstructions, anatomically-shaped prostheses (in the shape of a water droplet) will be used to best reproduce the natural shape of the breast before it was operated on.
Reconstruction using a prosthesis can be performed when the pectoral muscle and skin are of good quality because they will be used to cover the prosthesis.
On the other hand, when the muscle and skin have been damaged too much, reconstruction will be carried out using other techniques using tissues from other parts of the body such as the large dorsal muscle or the rectus abdominus muscle.
In addition to restoring breast volume, the reconstruction will finish off by reconstructing the areola and nipple in a second operation after the reconstructed breast has stabilised in volume.
This restored sense of harmony is a factor of well-being and self-confidence, whether the body is naked or clothed.

Reconstruction of the left breast by axillary anatomical prosthesis, with areola and nipple reconstruction by skin grafting. Also right breast symmetrisation by lifting
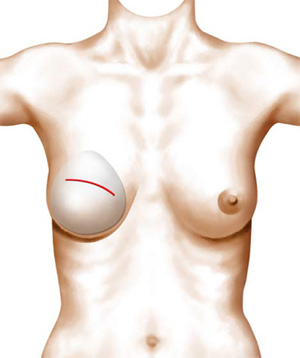
The prosthesis can be put in place through an axillary incision to avoid reopening the mastectomy scar.
Uses
For patients who want breast reconstruction using a prosthesis after a mastectomy (removal of the breast), it will be necessary to ensure that the covering tissues (pectoral muscle and skin) are of sufficient quality and thickness to allow adequate coverage of the prosthesis.
A breast prosthesis is made up of an outer shell and its contents.
There are different types of prostheses, which vary with different shell textures, different types of filling, shape, volume and projection, making it possible to adapt these to the anatomy of each individual patient. The different types of prostheses are described in chapter 160; Breast augmentation with prosthesis.
In the majority of reconstructions, rather than using round-shaped prostheses, we use anatomically shaped prostheses (water droplet shape) with silicone gel fillings, as these best reproduce the natural shape of a breast before it was operated on, the shape of the breast being entirely determined by the shape of the prosthesis.
In addition, to improve a contoured look and feel of the prosthesis and the reconstructed breast, it is preferable to use a prosthesis with a reinforced shell made from thick polyurethane foam as this will give more softness when covered by the skin and muscle.
Some reconstructions using a prosthesis will require tissue expansion beforehand if the skin and muscle are too tight to accommodate the contours of the prosthesis. A temporary prosthesis called a "skin expander" is first used and this is initially smaller in volume but is gradually inflated, stretching the skin until it will sufficiently cover the desired final volume. The final prosthesis is put in place during a second operation.
Consultation
During the first consultation, it is essential that you openly express what bothers you and what you would like to improve. Do not be afraid to ask any questions, including expressing your fears and expectations. Everyone has a different body shape, psychology and expectations. These are not the same and there is no standard to apply.
After you have explained your motivations, I will examine you and offer one or more solutions, taking into account your expectations, your anatomy, respecting your identity and the harmony of your physique.
During the first consultation, I will evaluate the type of prosthesis to use and the right volume.
So you can visualise the desired result, I will show you photos of surgical results from cases similar to yours to enable you to understand the objective of the intervention and the type of prosthesis and its volume.
It is essential that you and I have a good understanding when deciding to operate and to determine the technique to use from among those I can offer.
I will then give you all the information on the techniques proposed along with the information sheets from the Société Française de Chirurgie Plastique Reconstructrice et Esthétique (French Society of Plastic, Reconstructive and Cosmetic Surgery) as well as a detailed estimate of the costs for the options chosen. You will then be able to move your project forward and get ready for a second consultation when you will be able to ask any additional questions to help you make a decision and prepare for the operation.
Before the procedure
You will need a consultation with the medical-surgical team who treat breast cancer to determine the appropriate time for reconstruction. Then, we will carry out the pre-operative examinations deemed necessary by all practitioners concerned.
In the case of a general anaesthetic, you will need a consultation with the anaesthetist in the weeks preceding the operation and at least 48 hours before.
You will need to shave your armpits a few days before the operation if the prosthesis is being inserted using the axillary route (see Technique).
You will be prescribed a bra to buy, which is specifically suited to post-operative restraint. You must bring this on the day of the operation to be worn the end of the operation.
Recommendations
No medications containing aspirin or anti-inflammatories can be taken within 10 days of the procedure.
For a general anaesthetic, you will have to fast strictly for 6 hours before the operation (do not eat anything, chew gum, eat sweets or smoke).
Smoking can cause scarring problems.
The procedure
Hospitalisation and the duration of the procedure:
Your stay in hospital is usually limited to the night following the operation.
The procedure lasts about 1.5 hours.
Type of anaesthetic
In most cases, the operation is carried out under general anaesthetic.
Technique
Before you go to the operating theatre, in your room, I will go over the precise goals with you as we agreed during the consultations. You can then always make recommendations and ask any questions. I will then draw the lines and marks on your skin to guide the operation and the lines of the incisions.
There are different insertion routes and positions for the prosthesis.
It is very common to use the mastectomy scar, which is generally located at the top of what will become the space for the prosthesis. The scar is then placed under maximum tension when covering the prosthesis. In my opinion, this weakens the coverage of the prosthesis, especially in the event of delayed healing.
For this reason, I prefer to use the axillary route by making an incision in the hollow of the armpit, which is a distance from the site of the prosthesis and is not subjected to any tension. Also, it is in a retro-pectoral position that allows better coverage of the prosthesis.
The axillary approach has many advantages in breast reconstruction with prosthesis:
-
It completely preserves the integrity of the tissues covering the prosthesis as these will not be cut when the prosthesis is introduced. Due to its lateral position behind the pectoral muscle, the axillary approach allows the pectoral muscle, the skin and the non-reopened mastectomy scar to be lifted together to form the cavity for the prosthesis.
-
It provides a natural look and feel and preserves all the potential elasticity of the tissues, which stays intact, as is needed to cover the increased volume.
-
It offers more stability to maintaining the prosthesis, which is located behind the tissues that remain intact.
-
It favours scar healing by avoiding the risks associated with the mastectomy scar reopening in a weakened area. This is particularly the case where the patient has had consecutive radiotherapy treatments and the scar is located at the maximum point of tension when covering the prosthesis.
The axillary approach creates a very discrete scar, hidden in the hollow of the armpit and kept within the area covered by hair.
The stitches are placed within the skin’s thickness (intradermal stitches) and are, therefore, invisible. These stitches are absorbable so they do not need to be removed.
At the end of the operation, a suction drainage is used to limit hematoma formation, a dressing is applied to the scar and a support bra is put in place to hold the prosthesis in the desired position.
After the operation
During the night and days following the operation, you may feel a painful sensation of tension in the area that was operated on, such as aches and pains, which may impede your mobility. These pains are moderate in a resting position and may require analgesics, which are given by drip if you are staying in hospital or can be taken as tablets at home. These post-operative pains will reduce and disappear within a few days of the operation.
The drainage will be removed and the dressing loosened the day after the operation. The dressing can be completely removed at the first post-operative check-up 4 days after the operation. However, the support bra must be worn day and night for one month.
As the stitches used are absorbable, they do not need to be removed. Placed internally within the skin’s thickness (intradermal stitches), they are invisible.
Swelling (oedema) and bruising around the thoracic area are usually very moderate and it takes about ten days for these to almost completely disappear.
You will need to take about 8 days off work in most cases.
Care
In addition to wearing a support bra day and night for 1 month, you should clean the scar daily with antiseptic.
You will need to arrange a follow-up visit 4 days after the procedure, then after 15 days, 1 month, 3 months, 6 months, 1 year and then once a year.
Recommendations
-
Do not raise your arms too high and avoid heavy physical exertion.
-
You may think about resuming sporting activities 1 month after the operation while wearing the support bra and limiting yourself to painless movements. However, intensive weight training using the chest area is strongly discouraged.
-
Driving can cause problems for 2 to 3 days if you have to make manoeuvres without power steering as well as simply manipulating the gear lever.
-
The recommended rest position is lying on your back, slightly raised if possible. You may also lie on your side but you must not lie on your front
-
Exposure to the sun: no direct exposure before 1 month and then exposure is allowed using a sun protection cream with a maximum sun protection factor. No exposure as long as you have bruising.
The result
The new shape of the breast is immediately visible and perceptible to the touch despite any swelling. Even if the shape is initially a little tight, it will soften in the weeks following the operation.
It takes 5 to 6 months for the tissues to heal around the prosthesis and for the breast to become supple and natural, regaining all its sensitivity.
Wound healing around the prosthesis takes place by forming a capsule, a flexible membrane that surrounds the prosthesis to isolate it from the surrounding tissues, allowing the prosthesis to be integrated as far as possible into the body.
Once the volume and shape of the reconstructed breast have stabilised, the areola and nipple can be reconstructed. There are different techniques and I usually use a local dermo-adipose skin flap to re-establish the nipple as well as a skin graft to re-establish the areola. After healing, these can be coloured using dermo-pigmentation, which gives perfect control of all shades of colours from pink to brown to reproduce the natural hue for each individual patient.
In addition to the aesthetic improvement that this operation brings, it also has a beneficial impact on the patient's personal well-being and development.
Risks and complications
Price range
The cost of the operation will depend on the procedure to be carried out, the duration of the operation, the type of anaesthetic and any hospital charges.
You may be covered by Social Security and, where relevant, by your mutual insurance company after prior agreement from the Medical Adviser of the Primary Health Insurance Fund.
A detailed estimate is given to you during the first consultation following the options you have chosen. You then have a minimum legal period of 15 days to consider your options and move your project forward.
The first consultation costs €50. The follow-up consultations before and after the operation are free.
The photographs on this page are to illustrate and complete the information given on the operations. They are merely for information purposes so you can see the goals, results and scars from the operation.
The likelihood of scarring and each patient’s individual anatomy are different. For this reason, therefore, the photographs on this site do not commit Dr. Benelli to providing all patients with a similar result.
The information given on a site is not sufficient in itself and a medical consultation is essential to get the right information for each individual case. For this, you will need to consult a surgeon qualified in Plastic Reconstructive and Aesthetic Surgery.