Breast augmentation with prosthesis
The purpose of breast augmentation is to obtain a new shape that improves the harmony between the breasts and the rest of the body, while maintaining the most natural look and feel possible.
This new harmony is a factor of well-being and self-confidence, whether the body is naked or clothed.
This operation is intended for women whose breasts are poorly developed or have undergone changes in volume due to pregnancy or weight loss, leading to sagging.
Breast augmentation by inserting prostheses is one of the most commonly performed cosmetic surgery operations in the world because it is very gratifying, leaves only a slight scar that is not very visible and requires only a day in hospital with a short recovery time.
There are many models of prostheses whose materials, content, volume, shape and projection will adapt to the individual anatomy of each patient.
A prosthesis is like an internal garment and must fit the body with the maximum levels of comfort and harmony. Under these conditions, the patient "forgets" that the prostheses are there and these become completely integrated as part of her natural body image.
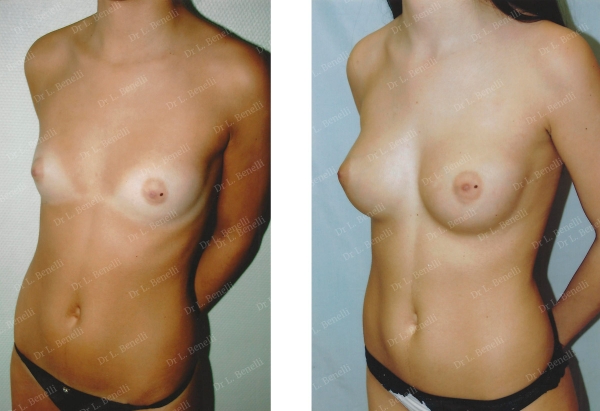
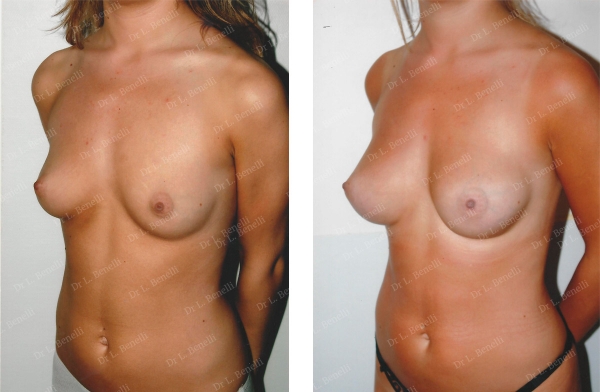
Anatomical prostheses using the axillary route without leaving a scar on the breast in the "dual plane" position. Result after 1 year
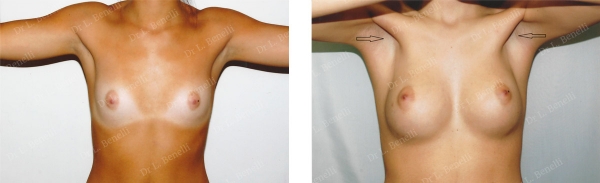
Same patient, no deformity in muscle contraction, discrete scars only in the armpit as indicated by the arrow
Uses
The operation meets varied expectations, depending on your age.
18-30 year olds:
These are young girls whose breasts have not developed, are under-developed or have developed asymmetrically while puberty has normally ended without any hormonal abnormality. Breast prostheses can be considered when puberty is completely over, the patient is physically an adult and the breast has been stable in size for more than 2 years.
30-45 year olds:
This category includes women who are suffering from breast sagging after one or more pregnancies or after significant weight loss. While the small volume was well supported when the breast was toned and firm, the sagging of the skin, especially in the areola and nipple, gives an empty breast appearance that can be perceived as a sign of ageing.
The 45 and over age bracket:
Around the time of the menopause, women experience tissue ageing and would like to keep a toned breast curve.
Breast reconstruction
Of course, women who want breast reconstruction following a mastectomy (breast removal) should be added to the profile of patients in each age group.
Each person arrives with a request for the correction of a particular defect that is particularly troublesome to them. The objective of the operation will be to correct this defect as a priority by assessing whether it may be appropriate to correct other associated defects to have a well-balanced, natural result that meets expectations.
So, depending on the insights gained during the first consultation, the operation could possibly be combined with other procedures, notably a breast lift aimed at breast enhancement for empty and sagging breasts, breast correction, inverted nipplesor an areola reduction. This can be done during the same intervention or at another time.

Breast lift by inserting axillary prostheses without a scar on the breast and simultaneous abdominal plastic surgery
Consultation
During the first consultation, it is essential that you openly express what bothers you and what you would like to improve. Do not be afraid to ask any questions, including expressing your fears and expectations. Everyone has a different body shape, psychology and expectations. These are not the same and there is no standard to apply.
After you have explained your motivations, I will examine you and offer one or more solutions, taking into account your expectations, your anatomy, respecting your identity and the naturalness of your appearance.
During the first consultation, I will evaluate the technique I will use, the type of prosthesis and its volume.
So you can visualise the desired result, I will show you photos of surgical results from cases similar to yours for you to understand the objective of the intervention, according to the form and volume used.
It is essential that you and I have a good understanding when deciding to operate and to determine the technique to use from among those I can offer.
I will then give you all the information on the techniques proposed along with the information sheets from the Société Française de Chirurgie Plastique Reconstructrice et Esthétique (French Society of Plastic, Reconstructive and Cosmetic Surgery) as well as a detailed estimate of the costs for the options chosen. You will then be able to move your project forward and get ready for a second consultation when you will be able to ask any additional questions to help you make a decision and prepare for the operation.

Anatomical prostheses using the axillary method without a scar on the breast in the "dual plane" position. Result after 1 year
What is a breast prosthesis?
A breast prosthesis is a volume substitute and aims to create a similar curve, look and feel of a breast, that has not been operated on, in a standing position, lying down and without contracting the muscles.
A breast prosthesis consists of an outer shell and its contents.
There are different types of prostheses that will vary in the texture of the shell, the type of filling, shape and volume.
What are the different types of breast prostheses?
Texture of the outer shell:
The shell is made of soft silicone. It can be smooth, textured, micro-textured, or covered with polyurethane foam. Choosing the right type of outer texture will be based on your anatomy.
Filling contents:
-
Silicone gel, which can be more or less flexible,
-
Saline solution,
-
Hydrogel (water and sugar).
Saline prostheses are known as "inflatable" because they are filled by the surgeon during the operation by injecting saline through a filling valve. Silicone gel or hydrogel prostheses are pre-filled by the manufacturer.
Hydrogel prostheses (water and sugar) using the axillary route without scar on the breast, dual plane position. Result after 1 year
Form
The shape of the prostheses is either round (hemispherical) or anatomical (drop-shaped).
With these different forms that are equal in volume, the ratio between the base of the prosthesis and its top can also vary: there are prostheses with a low projection (wide base) or a high projection (narrow base).
The profile and projection are designed to adapt to the different anatomical shapes of the thorax.

Anatomical prostheses using the axillary method without a scar on the breast in the "dual plane" position, correcting rib and sternum contour irregularities (Pectum Excavatum). Result after 1 year
Volume
The same prosthesis models have different volumes that allow a precise match with the desired increase.
Before the procedure
Pre-operative examinations should be performed:
-
Breast ultrasound and/or mammography to check breast health. These will allow any anomalies to be picked up and these may be treated during the operation or may possibly lead to additional pre-operative examinations.
-
A blood test.
If you have a general anaesthetic, you will need a consultation with the anaesthetist in the weeks preceding the operation and at least 48 hours before.
You need to shave your armpits a few days before the operation if the prosthesis is inserted using the axillary route (see Technique).
You will be prescribed a bra to buy, specifically for post-operative support. You must bring this with you on the day of the operation to be worn at the end of the operation.
Recommendations
No medication containing aspirin or anti-inflammatories should be taken within 10 days of the procedure.
For general anaesthetic, you will have to fast strictly for 6 hours before the operation (do not eat anything, chew gum, eat sweets or smoke).
Tobacco consumption should be stopped or reduced as much as possible during the month before and month after the procedure. Tobacco can cause scarring problems.
The procedure
Hospitalisation and the duration of the procedure
Your stay in hospital is usually limited to the night following the operation. Same-day discharge is also possible after a few hours of monitoring following the operation. During the night, painkillers and analgesics are given by drip if you are staying in hospital or are taken as tablets at home. Going home the next day, you will need to wear a simple specially-adapted support bra.
The duration of the procedure is about 1.5 hours.
Type of anaesthetic
In most cases, the operation is performed under general anaesthetic.
Technique
Before you go to the operating theatre, in your room, I will go over the precise goals with you that we agreed during the consultations. You can then always make recommendations and ask any questions. I will then draw the lines and marks on your skin to guide the operation and the lines of the incisions.
The prosthesis can be inserted using different methods and placed in different positions, depending on the anatomy of the patient.
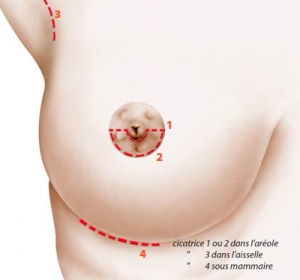
The different ways of insertion of the prosthesis:
The axillary route, making an incision in the hollow of the armpit,
The areolar route, making an incision around the lower half of the areola,
The sub-mammary route, making an incision in the sub-mammary fold.
The choice of the insertion route is determined by the anatomy of the patient and the shape and volume of the prosthesis.
The axillary route:
It has the advantage of not creating a scar on the breast and, instead, there is a discreet scar hidden in the hollow of the armpit and limited to the area covered by hair.
This also means the mammary gland does not have to be cut, keeping all the tissues that cover the prosthesis intact. The tissues are moved to one side using the axillary approach and a cavity is created for the prosthesis to go into.
Preserving the integrity of the tissue also conserves all its elasticity, which is needed for the increase in volume, contributing to a natural feel.
This procedure requires special instrumentation (special scrapers and sometimes endoscopy equipment).
Use: the axillary method is used as much as possible because it is the best way to cover the prosthesis with the tissue and avoids having to cut these. This is particularly important when a patient is thin and does not have much tissue coverage over the prosthesis; it is then preferable to preserve the integrity of these tissues.
The areolar route:
This has the advantage of direct visual control of the tissues and the area of separation.
On the other hand, it has the disadvantage of creating a scar on the areola. However, this is discreet and blends in with the areola that is coloured. The other disadvantage is that the mammary gland is severed along with the retro-areolar tissues, which can sometimes heal in a retractile fibrous manner that deforms the contour of the areola.
Use: The areolar approach is used when it is necessary to dissect the prosthesis compartment, giving the surgeon direct visual control of this procedure, in particular in the following cases:
-
Resuming prosthesis surgery that had unsatisfactory results,
-
Changing the position of the original sub-mammary fold,
-
When an areola reductionis carried out in addition to fitting the prostheses,
-
When the breasts are empty and sagging and a breast lift is being performed along with fitting the prostheses; in this case, the scar will go around the entire areola ("Round Block" technique) and not just the lower edge.
The submammary route:
We use this very rarely because it creates a visible scar in the sub-mammary fold, especially when lying down. In addition, the scar is located just where the prosthesis rests on the lower part of the breast, which weakens the scar and the prosthesis covering in a place where the tissues are very thin. It is basically used when repeating the first operation that was carried out using this method so another scar is not created.
For all these reasons, I generally prefer the axillary route with a discreet scar in the area covered by hair at the bottom of the armpit.
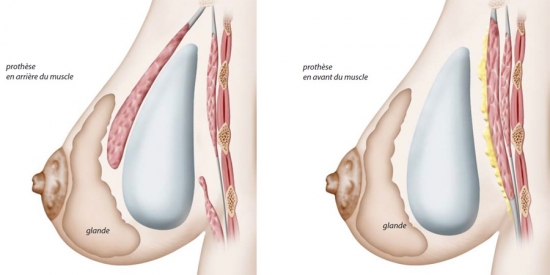
The different positions for the prosthesis:
-
Retro-glandular position: directly behind the mammary gland,
-
Retro-pectoral and retro-glandular ("dual plane") position: behind the pectoralis major muscle for the upper part of the prosthesis, the lower part is directly behind the mammary gland because the lower part of the pectoralis major will have been removed.
The retroglandular position:
This has the advantage of being easier to access because, behind the mammary gland, there is a natural space where the prosthesis can be placed.
The disadvantage is that the prosthesis has a more superficial level of cover, which then makes it more visible and palpable, especially when the patient is thin and the weight of the prosthesis is directly within the breast cavity, which can increase the likelihood of the breast collapsing by distending the skin.
The "Dual Plane" position:
This has the advantage of using the pectoral muscle as a cover for the prosthesis, which gives it a more natural look and feel, especially when the patient is thin.
Because there is a partial detachment of the pectoral muscle, its disadvantage is that it potentially causes more painful post-operative outcomes than with a simple retroglandular detachment.
Whatever technique is used, the stitches are placed within the skin’s thickness (intradermal stitch) and are invisible. These stitches are absorbable so they do not need to be removed.
At the end of the operation, a suction drainage is used to limit hematoma formation, a dressing is applied to the scar, and a support bra is put in place to hold the prostheses in the desired position.
After the operation
During the night and days following the operation, there may be a painful sensation of tension in the area that was operated on, such as aches and pains, which may impede your mobility. These pains are moderate in a resting position and may require analgesics that are given by a drip during your stay in hospital or are taken as tablets at home. These post-operative pains will diminish and disappear within a few days of the operation.
The drainage will be removed and the dressing loosened the day after the operation. The dressing will be completely removed at the first post-operative check-up 4 days after the operation. However, the support bra must be worn day and night for one month.
As the stitches used are absorbable, they do not need to be removed. Placed internally within the skin’s thickness (intradermal stitches), they are invisible.
Swelling (oedema) and bruising of the thoracic area are usually very moderate and it takes about ten days for them to disappear almost completely.
You will need to take 4 to 5 days off work in the majority of the cases.
Care
In addition to wearing a support bra day and night for 1 month, scars should be cleaned daily with an antiseptic.
You will need to arrange a follow-up consultation 4 days after the procedure, then after 15 days, 1 month, 3 months, 6 months, and 1 year, then once a year.
Recommendations
-
Do not raise your arms too high and avoid heavy physical exertion.
-
You may resume sporting activities 1 month after the operation by wearing a support bra and limiting yourself to painless movements. However, intensive weight training using the chest area is strongly discouraged.
-
Driving can cause problems for 2 to 3 days if you need to make manoeuvres without power steering or when simply moving the gear lever.
-
The recommended rest position is lying on your back, slightly raised if possible. You may also lie on your side but you must not lie on your front.
-
Exposure to the sun: no direct exposure before 1 month then exposure is allowed using a sun protection cream with a maximum sun protection factor. No sun exposure while you have bruising.
-
Pregnancy and breastfeeding: a prosthesis placed behind the retro-pectoral or pre-pectoral muscle is not in contact with the mammary gland, so there is no risk in the case of breastfeeding. However, it is advisable to wait 6 months before considering a pregnancy so that the breast has settled into its final form.
The result
The new shape of the breasts is immediately visible and perceptible to the touch despite any swelling. Even if the shape is initially a little hard, it will soften in the weeks following the operation.
It takes 1 to 3 months for the tissues to heal around the prosthesis and for the breast to be supple and natural and to regain all its sensitivity.
The healing around the prosthesis takes place to form a capsule, a flexible membrane that will surround the prosthesis and isolate it from the surrounding tissues, allowing it to be integrated into the body as much as possible.
In the long term, the result will be stable and sustainable.
The average life of a breast prosthesis was estimated to be 10 years but, for the new generations of prostheses, manufactured to higher strength standards than before, the average life should be longer.
Over time, the prosthesis undergoes normal wear and tear that will cause it to lose its ability to be waterproof. If leakage takes place on one of the prostheses, usually both prostheses have to be changed.
Leakage manifests itself in different ways, depending on the filling material used in the prosthesis:
-
For saline prostheses, the leak will quickly cause the prosthesis to deflate and therefore a loss of volume and breast sagging due to the natural elimination of saline by the body. There is no risk to the body from this leak.
-
For hydrogel prostheses (water and sugar), the leak temporarily causes a slight swelling of the breast because the sugar contained in the hydrogel will cause an influx of water for a few days. Then, the body will gradually eliminate the water and sugar, leading to a loss of breast volume. There is no risk to the body from this leak.
-
For silicone gel prostheses, the leaking seal may not initially be felt by the patient because the silicone is not reabsorbed by the body and the gel, by its cohesive nature, does not tend to come out of the shell of the prosthesis. On the contrary, the liquid naturally present in the capsule created by the body around the prosthesis enters and mixes with the silicone gel inside the prosthesis. The breast does not suffer any loss of volume. In some cases, there may instead be a swelling reaction in the breast. This loss of tightness can be detected by the patient, who notices a change in the sensations of the tissues surrounding the prosthesis (slight swelling, unusual pain or sensations, change in breast consistency, etc.) or during the annual check-up when feeling the breast. In case of doubt, additional examinations will then be carried out, with an initial ultrasound which is a simple and effective examination to detect a loss of the watertight aspect of the prosthesis and which can be repeated as often as necessary without any inconvenience.
Regardless of the lifespan of the prosthesis, breast volume remains stable over the long term. However, the shape and position of the breasts will evolve over time due to the natural ageing process, which also depends on the quality of tissue support and breast volume.
In addition to an aesthetic improvement, this operation has a beneficial impact on the patient's personal well-being and development.
Risks and complications
Price range
The cost of the operation will depend on the procedure to be carried out, the duration of the operation, the type of anaesthetic and any hospital charges.
If the reason for the operation is purely cosmetic, you cannot get any reimbursement through a Social Security claim. On the other hand, if it is for reconstructive purposes, you may be covered by Social Security and, if necessary, by your mutual insurance company.
A detailed estimate is given to you during the first consultation according to the options you have chosen. You then have a minimum legal period of 15 days to consider your options and move your project forward.
The first consultation costs €50. The follow-up consultations before and after the operation are free.
The photographs on this page are here to illustrate and complete the information given on the operations. They are merely for information purposes so you can see the goals, results and scars from the operation.
The likelihood of scarring, and each patient’s individual anatomy, are different. For this reason, therefore, the photographs on this site do not commit Dr. Benelli to provide all patients with a similar result.
The information given on a site is not sufficient in itself and a medical consultation is essential to get the right information for each individual case. For this, you will need to consult a surgeon qualified in Plastic Reconstructive and Aesthetic Surgery.